What is COVID-19 and How is it Related to TCD?
Covid-19, also called Coronavirus, is a newly identified virus that causes contagious disease. The Coronavirus led to a worldwide pandemic with respiratory illness and cerebrovascular diseases.
The Covid-19 pandemic became internationally widespread in early 2020. This contagious disease was initially thought to affect only respiratory illness and pulmonary function, but very quickly, it became evident that this disease is primarily a vascular disease with detrimental effects on the complete cardiovascular circulation. The cerebrovascular circulation is of primary interest because it has been shown that the incidence of stroke resulting from Covid-19 has increased, and particularly alarming is the fact that young adults became susceptible to stroke.
It is evident that cerebral embolization is a high-risk factor for stroke and neurological deficits.
How to use TCD for COVID-19
Transcranial Doppler (TCD) is the ideal and preferred non-invasive bedside modality for identifying and quantifying embolic events in the cerebral circulation, particularly in the Middle Cerebral artery (MCA).
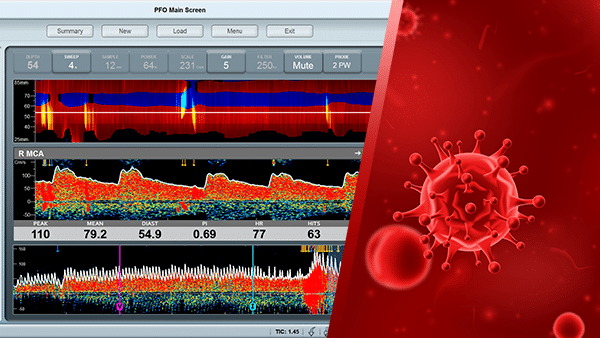
The embolic events are clearly seen in the Doppler spectrum and power m-mode displays and have a unique Doppler sound, which is based on the embolic characteristics.
Patients with a Patent Foramen Ovale (PFO) are particularly affected by micro-emboli from venous sources.
The shunt between the right and left atriums of the heart in those patients may cause venous emboli to be re-directed directly to the brain, thus increasing the potential for ischemic cerebrovascular events.
In addition, potential cerebro-arterial stenosis or clot will affect the arterial flow velocities, and TCD can quickly diagnose abnormal flow conditions in the cerebral circulation, including the arteries that comprise the Circle of Willis.

Monitoring Headset
Perform Bedside Monitoring Bilaterally

Robotic Probe
Fast, Stable, and Comfortable Monitoring
Using Dolphin for COVID-19
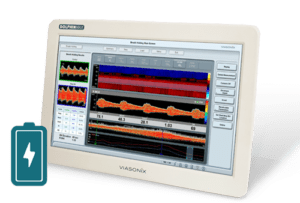
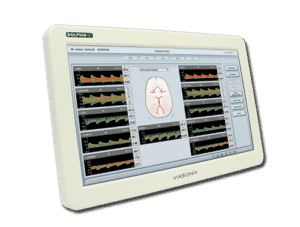
The Dolphin transcranial Doppler system has dedicated unilateral or bilateral HITS (High-Intensity Transient Signals) detection protocols that are effective in identifying cerebral emboli and micro-bubbles. The advanced HITS analysis options count all suspected emboli automatically and allow the use of advanced analysis tools for further examination and determination of each suspected embolic event.
Special PFO protocols are provided for quick determination of the existence of a shunt between the right and left atriums, as well as count the HITS in order to determine the anatomical severity of the PFO.
The Monitoring protocols in the Dolphin provide long-term bedside monitoring of the cerebral circulation with a special dedicated monitoring headgear. The blood flow velocities and different pulsatility indices are continuously displayed as parameter trends as a function of the monitoring session. Thus, the effects of medication, special medical conditions, or clinical interventions on the cerebral blood flow are quickly detected and serve for improved patient clinical outcomes.
Expected Results
One objective of TCD measurements is to determine whether the mean flow velocity in the cerebral arteries is significantly different from normal flow velocity values in the cerebral circulation.
Another objective is to identify and count emboli during monitoring of the MCA in order to determine the risk for developing stroke or other neurological conditions.
PFO testing provides an immediate diagnosis of the existence of a Patent Foramen Ovale and based on the embolic count, the magnitude of the PFO can be assessed.
Selected Literature
Transcranial Doppler Ultrasound Evidence of Active Cerebral Embolization in COVID-19, Ayush Batra et al., Journal of Stroke and Cerebrovascular Diseases, Vol. 30, No. 3 (March), 2021: 105542
Acute Stroke in a Young Patient with Coronavirus Disease 2019 in the Presence of Patent Foramen Ovale, Muddasir Ashraf and Sulaiman Sajed, Cureus 12(9): e10233, September 03, 2020
Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19, Maximilian Ackermann et al., N Engl J Med 2020;383:120-8
Pulmonary Vascular Dilatation Detected by Automated Transcranial Doppler in COVID-19 Pneumonia, Alexandra S. Reynolds et al., American Journal of Respiratory and Critical Care Medicine Volume 202 Number 7, October 1 2020
Neurological Complications and Noninvasive Multimodal Neuromonitoring in Critically Ill Mechanically Ventilated COVID-19 Patients, Denise Battaglini et al., Frontiers in Neurology, November 2020, Volume 11, Article 602114
COVID-19 and cerebrovascular diseases: a comprehensive overview, Georgios Tsivgoulis et al., Ther Adv Neurol Disord 2020, Vol. 13: 1–18
COVID-19 – A vascular disease, Hasan K. Siddiqi, Peter Libby, Paul M Ridker, Trends in Cardiovascular Medicine 31 (2021) 1–5
Incidence of thrombotic complications in critically ill ICU patients with COVID-19, F.A. Klok et al., Thrombosis Research 191 (2020) 145–147
Disclaimer of Information & Content
The content of Viasonix Ltd. website is for information only, not advice or guarantee of outcome. Information is gathered and shared from reputable sources; however, Viasonix Ltd. Management is not responsible for errors or omissions in reporting or explanation. No individuals, including those under our active care, should use the information, resources or tools contained within this self-diagnosis or self-treat any health-related condition. Viasonix Ltd. Management gives no assurance or warranty regarding the accuracy, timeliness or applicability or the content.