In the whirlwind of medical technology, automation is a term that often pops up. It’s associated with convenience, speed, and simplicity for both patients and healthcare professionals.
But let’s take a moment to discuss automated Ankle Brachial Pressure Index (ABPI) devices – instruments poised to capture a significant share of the cost-effective Peripheral Arterial Disease (PAD) diagnosis market.
ABI is a key diagnostic tool for PAD, a condition that can complicate leg ulcer management. The traditional, manual method of measuring ABPI can take a full hour and may be uncomfortable for patients.
So, you might think that automated ABPI devices, with their promise of speed and ease of use, are the answer. But is this really the case?
What are these Automated ABPI Devices?
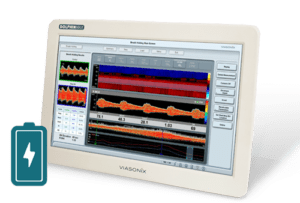
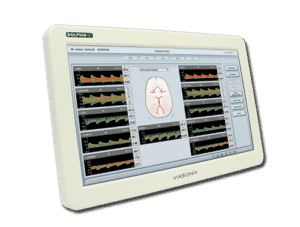
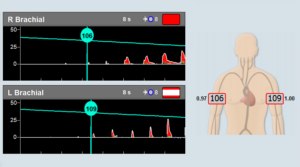
Automated ABPI devices use oscillometric technology to detect systolic blood pressures. They typically consist of a central unit and multiple cuffs that wrap around the patient’s limbs.
Once activated, the device automatically inflates and deflates the cuffs, simultaneously measuring blood pressure in all four limbs.
Obviously, the appeal of these devices lies in their convenience. They reduce the manual labor involved in the process, making it less cumbersome for healthcare professionals and potentially less uncomfortable for patients.
However, as we will discuss, the usage of these devices in the clinical setting is not without concerns and challenges.
The Evidence Gap
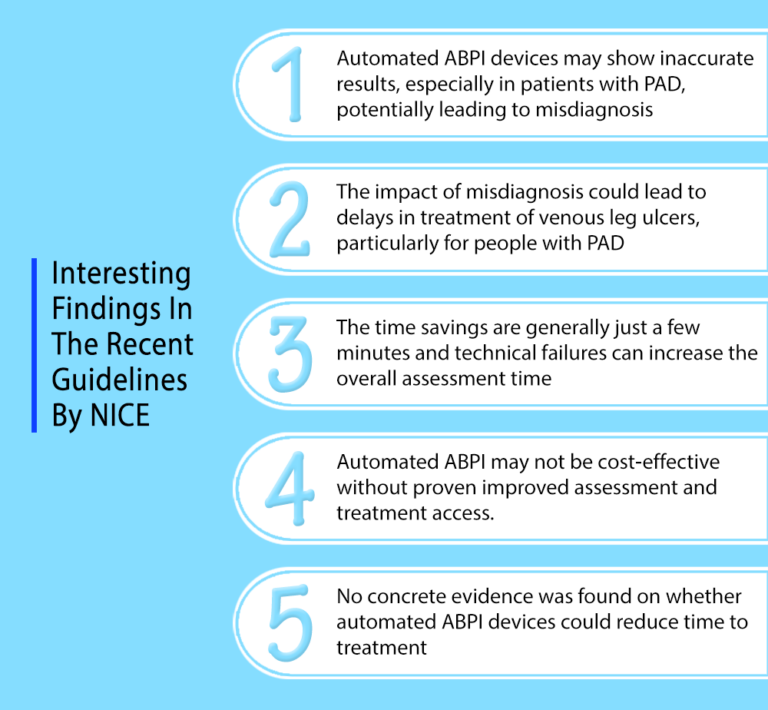
While the benefits of automated ABPI devices seem evident, there’s a significant problem. According to a recent National Institute for Health and Care Excellence (NICE) guideline published on 24 May 2023, there isn’t enough clinical evidence to back up these claims.
Although automated ABI devices are available in the market, studies have shown that they may not be as accurate as Doppler ultrasound. Most of the studies conducted to date were on individuals without leg ulcers. That leaves us in the dark about the effectiveness of these devices in the demographic that may need them most.
The Uncertainty of Misdiagnosis
There’s also the risk of misdiagnosis. What happens if these devices give inaccurate results? What does that mean for patients and their treatment?
Let’s consider Jane, a hypothetical patient with a leg ulcer. If she’s wrongly diagnosed as negative for PAD due to an inaccurate reading from an automated ABPI device, her treatment for venous leg ulcers could be delayed. Worse yet, she could be subjected to compression therapy that, in her case, could be harmful.
The Falcon/PRO Solution: The Power of Doppler and PPG
Doppler ultrasound remains the gold standard for ABI measurement. It allows healthcare professionals to visualize blood flow patterns and identify any abnormalities or blockages that may be missed by automated devices. This level of detail can help diagnose PAD earlier and more accurately, leading to better treatment outcomes for patients.
Furthermore, Doppler ultrasound can detect subtle changes in blood flow over time and track changes before and after treatment. This level of monitoring cannot be achieved with automated devices, which only provide a snapshot of blood pressure at a single moment.
“Clinical experts highlighted the value of information provided by Doppler waveform signals in these situations.
Devices that do not provide Doppler waveform signals may provide information about the quality of arterial circulation in the ankles, but there is uncertainty about whether these alternative outputs are comparable with Doppler waveform signals”.
From the National Institute for Health and Care Excellence (NICE) guideline published on 24 May 2023.
In the face of these challenges, there is a viable solution that combines the accuracy of Doppler with the convenience of automation. The Falcon/PRO offers a complete vascular diagnostic system that measures ABPI and segmental pressures using Doppler: the gold standard in vascular measurement according to international guidelines such as those published by the Society for Vascular Ultrasound. For Toe Brachial Index (TBI) measurements, it utilizes Photoplethysmography (PPG), which is widely accepted as a valid TBI measurement.
With this combination of technologies, the Falcon/PRO addresses the concerns of diagnostic accuracy while offering the benefits of an automated device. This solution is ideal for those who prioritize precise diagnosis without compromising on convenience and ease of use.
Navigating with Caution
In closing, the recent publication is an important guideline. It’s crucial to remember that in the realm of medical technology, patient safety and effective treatment must always come first.
As we continue to explore and develop new technologies, let’s do so with caution and rigor, ensuring that we never compromise on the well-being of our patients.
As always, before incorporating new technologies into healthcare practices, it’s important to consult with relevant professionals and guidelines. The world of medical technology is an exciting place, but it requires careful steps.
For more information, please leave us a message.