What is Sickle Cell Disease?
Sickle Cell Disease (SCD) is a hereditary disorder of the blood caused by abnormal form of hemoglobin, which causes distorted (sickled) red blood cells. It is associated with a high risk of stroke, particularly in the early years of childhood.
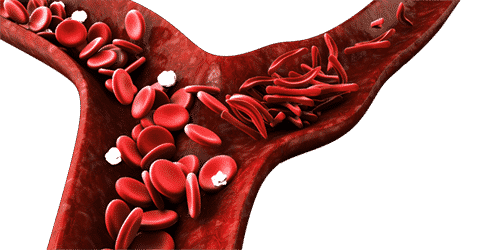
These “sickled” red blood cells are less flexible and have a tendency to stick together, leading to blockages in blood vessels. As a result, the main risk of Sickle Cell Disease is the potential for vascular constriction or occlusion, which may lead to subclinical infarction, acute stroke, and hemorrhage.
From a genetic perspective, SCD is primarily inherited when a child receives two copies of the hemoglobin S gene, one from each parent. However, individuals with only one copy of the gene may have a condition called sickle cell trait, which usually does not cause symptoms but can be passed on to their offspring.
Symptoms of Sickle Cell Disease:
- Pain Crises: SCD can cause episodes of severe pain called pain crises. These episodes occur when sickled red blood cells block blood flow in the small blood vessels.
- Anemia: The abnormal shape of the red blood cells can lead to a shortage of healthy red blood cells, causing anemia.
- Fatigue: Anemia can result in fatigue and weakness due to reduced oxygen-carrying capacity in the blood.
- Jaundice: The breakdown of sickled red blood cells releases a substance called bilirubin, leading to yellowing of the skin and eyes (also known as jaundice).
- Organ Damage: The repeated blockages and reduced blood flow can damage organs, especially the spleen, kidneys, and liver.
Children before the age of 20 with SCD are particularly susceptible and are at high risk of developing ischemic stroke. Blood transfusion in these cases can help to reduce the risk of stroke significantly.
High Risk of Stroke in Sickle Cell Disease
One of the most critical complications of SCD is the increased risk of stroke, especially in children. Children with SCD before the age of 20 are particularly susceptible to stroke, making early detection and preventive measures crucial.
Regular and routine Transcranial Doppler (TCD) screening is crucial for patients with SCD to identify those at risk of developing stroke. TCD is a non-invasive and safe diagnostic tool that measures blood flow velocities in the brain’s blood vessels. It is the primary method used to assess the risk of stroke in SCD patients.
Why TCD is Needed Routinely for SCD Patients:
- Early Detection of Abnormal Blood Flow: TCD allows healthcare professionals to detect abnormal blood flow patterns in the brain, which can indicate an increased risk of stroke. By identifying these patterns early on, medical interventions and preventive measures can be implemented to reduce the likelihood of stroke.
- Proactive Stroke Prevention: Routine TCD screening helps healthcare providers adopt a proactive approach to prevent strokes in SCD patients. Early identification of high-risk individuals allows for the implementation of appropriate therapies, such as blood transfusions or other medical interventions, to reduce the risk of stroke and its devastating consequences.
- Personalized Treatment Plans: TCD results provide valuable information about a patient’s specific risk of stroke. Healthcare providers can tailor treatment plans based on individual TCD findings, ensuring that patients receive the most suitable and effective preventive strategies.
- Long-Term Monitoring: Routine TCD screening enables ongoing monitoring of a patient’s stroke risk over time. This allows healthcare professionals to make necessary adjustments to the treatment plan as the patient’s condition evolves.
- Enhancing Patient Outcomes: Timely TCD screening and preventive interventions significantly improve patient outcomes by minimizing the risk of stroke and its potential complications, including permanent neurological damage and disability.
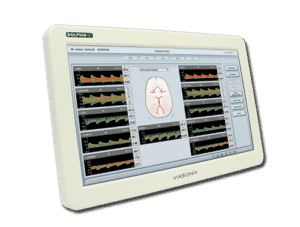
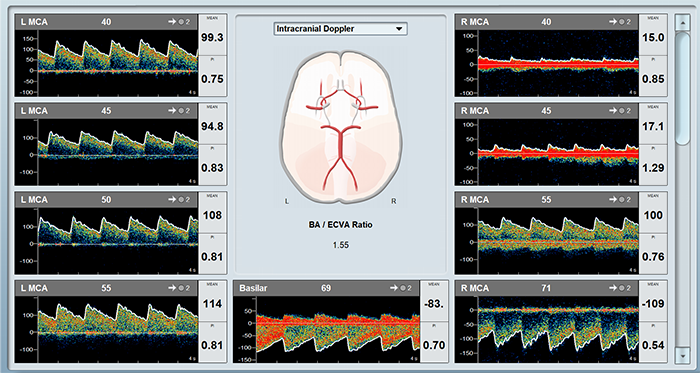
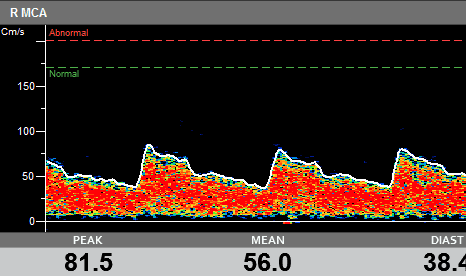
An example of a Sickle Cell measurement taken using Viasonix Dolphin system, showing automatic thresholds over the spectrum display.
How to use TCD for Sickle Cell Disease
Transcranial Doppler (TCD) is a key non-invasive modality in identifying the risk of stroke in SCD patients. Various scanning protocols for SCD are available, but in general, velocity measurements are made in the anterior and posterior circulations for detection of high or otherwise abnormal blood flow velocities.
Step 1: STOP Protocol
The most common established guidelines for Sickle Cell Disease testing is the “Stroke Prevention in Sickle Cell Disease” (STOP) study guidelines. These guidelines provide standardized protocols for using Transcranial Doppler (TCD) ultrasound to assess the risk of stroke in children with sickle cell anemia.
Step 2: Patient Preparation
Ensure the patient is comfortably positioned, preferably lying down, to minimize movement during the test.
Step 3: Select a TCD System
Select a suitable TCD system with a 2 MHz Doppler probe, known for its high-quality and ultra-sensitive blood flow detection. It is critical that the TCD system will display mean velocity in (Time Average Mean of the Maximum velocities) TAMM method.
Step 4: TCD System Setup
Configure the TCD system to the appropriate settings for SCD testing, including depth resolution and velocity scale, following the STOP guidelines.
Step 5: Scanning Protocol
Start by carefully scanning the anterior and posterior circulations of the brain to detect abnormal blood flow velocities associated with an increased risk of stroke.
In children, begin the Middle Cerebral Artery (MCA) scanning at a shallow depth, less than 40 mm, to obtain accurate velocity recordings. Track optimized velocity recordings along the vessel at a high depth resolution, with at least 2 mm depth increments.
Continue to perform scanning of other relevant blood vessels, such as the Anterior Cerebral Artery (ACA), Posterior Cerebral Artery (PCA), and distal Internal Carotid Artery (ICA), to assess blood flow velocities in these vessels.
Step 6: Analysis and Interpretation of Results
Collect the Doppler data during the scanning process to obtain velocity measurements in the cerebral blood vessels. Then, analyze the Doppler waveforms and parameters, including the TAMM, using the TCD system’s software.
Finally, compare the obtained velocity measurements with the STOP guidelines to determine the risk classification for the patient.
Important Note:
This step-by-step guide for performing a Sickle Cell Disease test is for informational purposes only. Healthcare professionals should rely on their expertise, clinical judgment, and institutional protocols for accurate administration and interpretation. Additional clinical information, patient history, physical examination, and other diagnostic tests may be necessary for comprehensive evaluation.

2 MHz Doppler Probe
High quality and ultra sensitive Doppler probe
Using Dolphin for SCD Test
The Dolphin TCD has a dedicated Sickle Cell Disease (SCD) examination protocol. The protocol is designed to meet the guidelines of the STOP (Stroke Prevention in Sickle Cell Disease) study:
- TAMM Method: The Dolphin displays all relevant Doppler parameters, including a Mean Velocity calculated with TAMM method, as required by the STOP protocol.
- Depth Control: The start-depth of the examinations is also allowing to start the vascular scanning at a shallow depth.Also, the incremental depth steps can be configurable to 2 mm per the STOP guidelines or at a much higher or lower resolution from 0.5 mm and up to 5 mm depth steps.
- Advanced Trends: The Dolphin software allows comprehensive trending abilities with options to correlate the TAMM results with hemoglobin and other external tests. When a patient visits again, the software pulls the patient history automatically and adds it to the report for a more accurate interpretation.
- Powerful M Mode Display: The phasic m-mode display is designed to quickly identify cerebral blood vessels, while the power m-mode display provides clear identification of transient high-intensity signals such as emboli passing through the artery.
- HITS Detection: The advanced and unique HITS processing capabilities of the Dolphin allow detailed analysis and view of each suspected embolic event, which may lead to ischemic stroke.
Cursors: It includes fixed velocity cursors that mark the normal and abnormal velocity thresholds per the guidelines.
Expected Results
The key guideline for TCD testing for SCD is the STOP (Stroke Prevention in Sickle Cell Disease) Study. According to the STOP classification of Transcranial Doppler results in children with sickle cell anemia:
| Range | Common Diagnosis |
|---|---|
| < 170 | Normal |
| ≥ 170 but < 200 | Conditional |
| ≥ 200 | Abnormal |
| Inadequate classification | Study was unable to be read |
Selected Literature
Stroke Prevention in Sickle Cell Disease (STOP) Study Guidelines for Transcranial Doppler Testing, Fenwick T. Nichols, Anne M. Jones, and Robert J. Adams, J Neuroimaging 2001;11:354–362
The Management of sickle Cell Disease, National Institutes of Health, Division of Blood Diseases and Resources, NIH Publication No. 02-2117, Revised June 2002
TCD and sickle cell disease, Fenwick T. Nichols III, Robert J. Adams, & Anne M. Jones, Chapter 7 in Cerebrovascular Ultrasound in Stroke Prevention and Treatment, Edited By Andrei V. Alexandrov, Blackwell Publishing, Inc., 2004
Assessment: transcranial Doppler ultrasonography: Report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Sloan MA et al., Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2004 May 11;62(9):1468-81
Stroke Prevention Trial in Sickle Cell Anemia (STOP): extended follow-up and final results, Margaret T. Lee et al., BLOOD, 1 AUGUST 2006, VOLUME 108, NUMBER 3
Transcranial Doppler screening in sickle cell disease: The implications of using peak systolic criteria, Lena N Naffaa, Yasmeen K Tandon, Neville Irani, World J Radiol 2015 February 28; 7(2): 52-56
Transcranial Doppler ultrasonography in neurological surgery and neurocritical care, Robert H. Bonow et al., Neurosurg Focus 47 (6):E2, 2019
Transcranial Doppler: Techniques and advanced applications: Part 2, Sharma AK, Bathala L, Batra A, Mehndiratta MM, Sharma VK, Ann Indian Acad Neurol. 2016 Jan-Mar;19(1):102-7
Transcranial Doppler, Review Article, Manish K. Marda, Hemanshu Prabhakar, J Neuroanaesthesiol Crit Care 2015;2:215-20
Disclaimer of Information & Content
The content of Viasonix Ltd. website is for information only, not advice or guarantee of outcome. Information is gathered and shared from reputable sources; however, Viasonix Ltd. Management is not responsible for errors or omissions in reporting or explanation. No individuals, including those under our active care, should use the information, resources or tools contained within this self-diagnosis or self-treat any health-related condition. Viasonix Ltd. Management gives no assurance or warranty regarding the accuracy, timeliness or applicability or the content.